Hall Ticket number :-1701006080
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs". This E log book also reflects my patient-centred online learning portfolio and your valuable comments on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Case Details
A 69 year old male, agricultural labourer by occupation hailing from panthangi has come to the hospital with the following complaints
1. SHORTNESS OF BREATH SINCE 20 DAYS
2. COUGH SINCE 20 DAYS
3. FEVER SINCE 4 DAYS
HISTORY OF PRESENT ILLNESS
The patient was apparently alright 20 days ago, then he developed Shortness of breath which was insidious in onset, MMRC grade 2-3 aggravated on Exertion and exposure to cold ,releived on taking rest. There is no history of breathlessness on lying down or Sleep disturbance due to SOB
He also complains of Cough with expectoration- sputum is mucoid, non blood stained, non foul smelling. No aggrevating factors, releived on rest.
He also complains of fever since 4 days which was insidious in onset, continuous in nature. No Chills and rigors. Fever was releived on taking medication.
Patient gives a history of loss of appetite and loss of weight and also dragging sensation in the right side of chest
The patient denies history of Nasal obstruction,nasal discharge, sore throat, hoarseness of voice , noisy breathing and chest pain
PAST HISTORY
No history of similar complaints in the past
No history of Diabetes,Hypertension,Asthma Tuberculosis,epilepsy, Thyroid problems
Personal history
Appetite :- Decreased
Diet :-mixed
Bowel and bladder :- regular
Sleep :- adequate
Addictions :- He smokes 4 beedis per day since 50 years. He takes alcohol occasionally.
Family history
No history of similar complaints in family
GENERAL PHYSICAL EXAMINATION
Patient is conscious, coherent and cooperative
Thin built and moderately nourished
Pallor :- Present
Icterus :- Absent
Cyanosis :- Absent
Lymphadenopathy :-Absent
Pedal Edema :-Absent
Vital signs
Temperature :- He is afebrile
Respiratory Rate :-22 cycles per minute
Pulse :-
Rate :-80 beats per minute
Rhythm :- Regular
Volume :- normal
Character :- normal
Condition of vessel wall :- Normal/soft
No radio radial or Radio femoral delay
Blood pressure :- 120/80 mmHg taken from Left arm ,measured in sitting position
SYSTEMIC EXAMINATION
The patient was examined in a well lit room after taking a valid informed consent after adequate exposure
RESPIRATORY SYSTEM EXAMINATION
Upper respiratory tract :- Normal
Examination of Chest
Inspection
The chest appears to be normal and bilaterally symmetrical
Trachea appears to be central in position
Apical impulse is seen in fifth intercostal space
No bony abnormalities of chest
Movements of chest with respiration appear to be reduced on the right side
No evidence of usage of accessory muscles for respiration
No scars and sinuses seen
No dilated veins are seen on the chest wall
Palpation
No local rise of temperature
No tenderness
All the inspectory findings are confirmed
Trachea is deviated towards right side (by 3 finger test)
Chest diameters
Transverse :- 27 cm
Anteroposterior :-20 cm
Movements of chest with respiration are reduced on right side
Apical Impulse :- 5th intercostal space 1 cm medial to mid clavicular line
Vocal fremitus -increased in Right suprascapular and right infraclavicular area
Percussion
The areas percussed include the supraclavicular, infraclavicular, mammary, axillary, infraaxillary, suprascapular, infrascapular areas.
Dull note was noted in Right infraclavicular and suprascapular areas
All other areas were resonant
Auscultation
Normal vesicular breath sounds heard
Diminished breath sounds in Right infraclavicular area and Right Suprascapular area
Fine crepitations heard in Right mammary and infra axillary area
Vocal resonance increased in right Infraclavicular and Right suprascapular areas
CARDIOVASCULAR SYSTEM-
Inspection-
No raised JVP
The chest wall is bilaterally symmetrical
No dilated veins, scars or sinuses are seen
Apical impulse or pulsations cannot be appreciated
Palpation-
Apical impulse is felt in the fifth intercostal space, 1 cm medial to the midclavicular line
No parasternal heave felt
No thrill felt
Percussion-
Right and left borders of the heart are percussed
Auscultation-
S1 and S2 heard, no added thrills and murmurs are heard
PER ABDOMINAL EXAMINATION :-
Soft and non tender
NO HEPATOSPLENOMEGALY
CENTRAL NERVOUS SYSTEM
Higher mental functions :-
- Patient is conscious ,coherent and cooperative
- Right handed individual
- Memory - immediate , short term and long term memory are assessed and are normal
- Language and speech are normal
Cranial nerves :- intact
Sensory system :-
Sensation right left
Touch felt felt
Pressure felt felt
Pain
-superficial felt felt
-deep felt felt
Proprioception
-joint position ✔ ✔
-joint movement ✔ ✔
Temperature felt felt
Vibration felt felt
Stereognosis ✔ ✔
Motor system
Right. Left
BULK
Upper limbs. N. N
Lower limbs N. N
TONE
Upper limbs. N. N
Lower limbs. N. N
POWER
Upper limbs. 5/5. 5/5
Lower limbs 5/5. 5/5
Gait :- Normal
Superficial and deep reflexes are elicited
No signs ssuggestive of cerebellar dysfunction
PROVISIONAL DIAGNOSIS
Right Upper lobe consolidation
Investigations
1.Sputum examination
Negative for acid fast bacilli
2. COMPLETE BLOOD PICTURE
Hb :- 11.7
TLC :- 15400
NEUTROPHILS:-82
EOSINOPHILS :-01
BASOPHILS :-00
LYMPHOCYTES:-10
MONOCYTES- 7
PCV:-34.7
RBC count :- 3.83 millions
PLATELETS:-2.83 lakhs
3. COMPLETE URINE EXAMINATION:
Normal
4. ABG
pH:-7.44
pCO2 :-34.3
pO2:-68.3
HCO3:-23.4
5. LIVER FUNCTION TESTS
TOTAL BILIRUBIN :-0.45
DIRECT BILIRUBIN:-0.17
AST :-28
ALT:-27
ALP:-202
ALBUMIN:-2.73
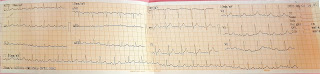
6.ECG
7. XRAY CHEST
No regional wall motion abnormality
Ejection fraction :-67
Mild diastolic dysfunction present
Treatment
1. Inj.Augmentin
2. Nebulisation with Duolin (BD)and budecort (TID)
3.Syp.Cremaffin 10 mL
4.Monitoring of vitals
5. Spo2 monitoring
6.Inj- PAN -40 mg OD
7.ASCORIL - CS ( 2 table spoons)



Comments
Post a Comment