I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Name :- Kattekola Sathwik
Roll no :-58
2017 batch
A 65 yr old farmer (man) hailing from Rural Nalgonda with a past history of Tuberculosis one year ago has presented with the complaints of
1. SHORTNESS OF BREATH SINCE 4 MONTHS
2. COUGH WITH EXPECTORATION SINCE ONE MONTH
3. CHEST TIGHTNESS SINCE 15 DAYS
HISTORY OF PRESENTING ILLNESS
The patient was apparently asymptomatic one year ago. Then he developed cough with expectoration with blood in sputum. He went to a local hospital and was diagnosed as TB after evaluation. He took the treatment for 5 months only .
Now from about 4 months he developed Grade 1 Shortness of breath (NYHA) which relieves on rest. There were no complaints of cough ,chestpain ,Orthopnea pedal edema that point of time
Then about from one month he is complained of cough with Greenish white expectoration.He says that the SOB was increasing after cough.
Then he has complained of chestpain from 15 days. He says that the chest pain increases after cough. He also says that the pain starts in the left side of the chest and then progresses to entire chest
No complaints of Orthopnea, PND
He also complains of Burning micturition and loin pain occasionally. No other urinary complaints
Past history :- No History of comorbidities
Personal history :-
Appetite :- Good
Diet :- Mixed
Bowel and bladder :- regular, Occasional burning micturition.
Sleep :- Adequate
Addictions:-
1. He is a chronic smoker since he was about 16 yrs of age . Smokes one packet of beedis per day
2. He is an occasional alcoholic
Family History:- No history of similar complaints
General examination
Patient was examined in a well lit room after obtaining valid informed consent and Adequate exposure
He was conscious, coherent, cooperative
Well oriented to time place person
Moderately built and nourished
Pallor :- Present
Icterus:- Absent
Cyanosis:- Absent
Clubbing :- present
Lymphadenopathy:-Absent
Pedal edema:- Absent
Appetite :- Good
Diet :- Mixed
Bowel and bladder :- regular, Occasional burning micturition.
Sleep :- Adequate
Addictions:-
1. He is a chronic smoker since he was about 16 yrs of age . Smokes one packet of beedis per day
2. He is an occasional alcoholic
Family History:- No history of similar complaints
General examination
Patient was examined in a well lit room after obtaining valid informed consent and Adequate exposure
He was conscious, coherent, cooperative
Well oriented to time place person
Moderately built and nourished
Pallor :- Present
Icterus:- Absent
Cyanosis:- Absent
Clubbing :- present
Lymphadenopathy:-Absent
Pedal edema:- Absent
Vitals
Temperature:- Afebrile
RR:-13cycles/min
Pulse :-76 bpm,regular,normal volume,normal character,vessel wall :-firm
BP :-120/80mmHg
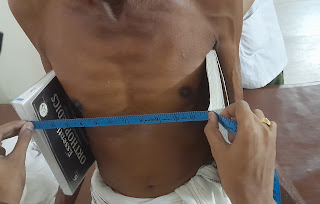
Clinical Images
Incidental finding in the patient- A swelling in the back and also the posterior aspect of right side of the neck.
Both of then were soft with with a smooth surface and soft in consistency without any signs of oongoing inflammation
The patient doesnt have any problem with these swellings...
Respiratory system
Inspection
Chest is bilaterally symmetrical
The trachea appears to be in centre
Apical impulse is not appreciated
Chest moves equally with respiration on both sides
No dilated veins, scars or sinuses are seen
Apical impulse is not appreciated
Chest moves equally with respiration on both sides
No dilated veins, scars or sinuses are seen
Palpation-
Trachea is felt in the midline
Chest diameters
- Anteroposterior diameter :-7 inches
- Transverse diamter:-12 inches
Apical impulse is felt in the fifth intercostal space 1cm lateral to mid clavicular line
Tactile vocal fremitus- appreciated
Percussion-
The areas percussed include the supraclavicular, infraclavicular, mammary, axillary, infraaxillary, suprascapular, infrascapular areas.
They are all resonant.
Auscultation-
Normal vesicular breath sounds are heard
No adventitious sounds
CARDIOVASCULAR SYSTEM-
Inspection-
The chest wall is bilaterally symmetrical
No dilated veins, scars or sinuses are seen
Apical impulse or pulsations cannot be appreciated
Palpation-
Apical impulse is felt in the fifth intercostal space, 1 cm lateral to the midclavicular line
No parasternal heave felt
No thrill felt
Percussion-
Right and left borders of the heart are percussed
Auscultation-
S1 and S2 heard, no added thrills and murmurs are heard
PER ABDOMEN
Inspection
• The abdomen is scaphoid
• Umbilicus is central
• No distention
• No engorged veins
• No visible pulsations
• No scars and sinuses
• Herinal orifices are free
Palpation
• No local rise of temperature and tenderness
• All Inspectory findings are confirmed
• On deep Palpation, Liver and spleen are not palpable
Percussion :-Tympanic note heard
Auscultation:- Bowel sounds appreciated
CENTRAL NERVOUS SYSTEM-
HIGHER MENTAL FUNCTIONS:
Patient is Conscious, well oriented to time, place and person.
All cranial nerves - Intact
No signs of meningeal irritation
Motor system
Right. Left
BULK
Upper limbs. N. N
Lower limbs N. N
TONE
Upper limbs. N. N
Lower limbs. N. N
POWER
Upper limbs. 5/5. 5/5
Lower limbs 5/5. 5/5
Superficial reflexes and deep reflexes are present, normal
Gait- normal
No involuntary movements
Sensory system- All sensations (pain, touch, temperature, position, vibration sense) are well appreciated
Provisional diagnosis
Post TB sequale with probable lung infection for further evaluation
Post TB sequale with probable lung infection for further evaluation
Investigations
Hemogram
• HB :-9.4
• Total WBC :- 8400 (N 77 L17 M5 E1)
• PCV :-31.5
• MCH :-21.2 MCHC :-29.8
• MCV :- 70.9
Hemogram
• HB :-9.4
• Total WBC :- 8400 (N 77 L17 M5 E1)
• PCV :-31.5
• MCH :-21.2 MCHC :-29.8
• MCV :- 70.9
• RDW :-18
• Platelets :-3.33 lakh
LFT
• Total bilirubin:- 0.44
• Direct bilirubin :- 0.15
• AST :-11
• ALT :-10
• A/G :- 0.63
Serum creatinine:-1.2
Blood urea:-31
Electrolytes
• Sodium:-141
• Potassium:-4.2
• Chloride :98
CUE
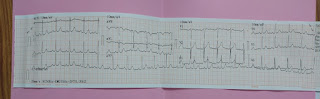
2D echo
Treatment
1. INJ AUGMENTIN 1.2G IV TID
2. INJ .PAN 40MG IV OD
3. T.MUCINAC AB TID
4. SYP. ASCOXIL TID 2 asp
5.NEB. with Duolin 6th hrly and BUDECORT 12TH HRLY
6. 4TH HOURLY VITALS MONITORING










Comments
Post a Comment