Hall Ticket number :-1701006080
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs". This E log book also reflects my patient-centred online learning portfolio and your valuable comments on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE DETAILS
A 26 old female, who is a home maker hailing from rural nalgonda has come to the hospital with following complaints
Lower back ache since 10 days
Fever since 5 days
Pain abdomen since one day
HISTORY OF PRESENTING ILLNESS
The Patient was apparently asymptomatic 10 days ago ..when she developed Lower back ache which was insidious in onset, continuous in nature, no aggravating factors, relieved on rest.
Thr patient also complained of fever since 5 days which was insidious in onset, remitting type ,associated chills and rigors, relieved on medication.
Now the patient also complains of Pain abdomen since a day which was in lower right quadrant of abdomen
The patient also complained of painless Passage of reddish coloured urine since a day
No history of burning micturition, frequency, urgency, shortness of breath pedal edema
PAST HISTORY
The patient gives a history of mitral valve replacement when she was 7 years old after which she is using Medication - ( ACITROM )
The patient has undergone lower segment cesarean section 7 months ago
No history of diabetes, Hypertension, asthma, epilepsy, tuberculosis
PERSONAL HISTORY
Appetite :- Good
Diet :- Mixed
Bowel and bladder :- Regular
Sleep :- Adequate
Addictions:- nil
Family History:- No history of similar complaints
General examination
Patient was examined in a well lit room after obtaining valid informed consent and Adequate exposure
She was conscious, coherent, cooperative
Well oriented to time place person
Moderately built and nourished
Pallor :- present
Icterus:- absent
Cyanosis:- absent
Clubbing :- absent
Lymphadenopathy:-absent
Pedal edema:- absent
Vitals
Temperature :- afebrile
Respiratory rate :-14 cycles per minute
Pulse:- 78 beats per minute, regular,normal in volume and character, no vessel wall thickening, no radioradial delay
Blood pressure :- 120/80 mmHg sitting position in right arm
Systemic examination
Per Abdomen
Inspection :-
Abdomen is scaphoid
All quadrants are moving equally with respiration
Umbilicus is central and inverted
There is a scar of lower segment Cesarean section
No visible peristlasis
No engorged veins
Hernial orifices are free
Palpation :-
All the regions were examined
Superficial palpation
No local rise of temperature
Tenderness in - Right lumbar region
Deep palpation
Liver,Spleen and kidney are not palpable
Percussion :-
Palpatory findings regarding liver span are confirmed
Tympanic note heard over the abdomen
Auscultation
Bowel sounds were normal
No venous hum
CVS :-
Inspection
The chest wall is bilaterally symmetrical
No dilated veins, or sinuses are seen
Midline scar is seen
Apical impulse or pulsations cannot be appreciated
No raised JVP
Palpation-
Apical impulse is felt in the fifth intercostal space, 1 cm medial to the midclavicular line
No parasternal heave felt
No thrill felt
Percussion-
Right and left borders of the heart are percussed
Auscultation-
S1 and S2 heard...
No added sounds or murmurs
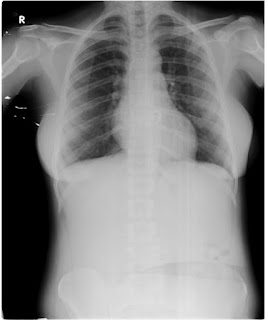
Respiratory system
Inspection
Chest is bilaterally symmetrical
The trachea appears to be in centre
Apical impulse is not appreciated
Chest moves equally with respiration on both sides
No dilated veins,sinuses are seen
Palpation-
Trachea is felt in midline
Chest moves equally on both sides on respiration
Apical impulse is felt in the fifth intercostal space 1cm lateral to mid clavicular line
Tactile vocal fremitus- appreciated
Percussion-
The areas percussed include the supraclavicular, infraclavicular, mammary, axillary, infraaxillary, suprascapular, infrascapular areas.
They are all resonant.
Auscultation-
Normal vesicular breath sounds are heard
No adventitious sounds
Central nervous system
Higher mental functions :- Normal
All cranial nerves are intact
No signs of meningeal irritation
Sensory, motor systems are normal
Provisional diagnosis
Acute pyelonephritis of Right kidney
INVESTIGATIONS
Complete blood picture
Hb:-10.1
TLC:- 13700
PCV 30.3
RBC count :-4.01 millions
MCV :-75fl
MCH :-25.2
Platelets :-3.14 lakhs
Complete Urine examination













Comments
Post a Comment