This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs". This E log book also reflects my patient-centred online learning portfolio and your valuable comments on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Name :- Kattekola Sathwik
Roll no 75
CHIEF COMPLAINTS:
Patient came with the chief complaints of low back ache since 4 months.
HOPI:
Patient was apparently asymptomatic 4 months back, then she developed pain which was insidious in onset and gradually progressive
Pain aggravated on bending forward and walking fast.
Relieved on lying down, but again aggravated after 5 hours of sleeping.
No H/O tingling sensations/ numbness
H/O slight difficulty in walking up and down the stairs.
Patient C/O low back pain more in winters
Patients routine-
Patient was housewife by occupation.
She has 2 kids who are studying in school.
She used to stay at home, have food and watches television.
6am- wakes up, and do some household works like sweeping, cooking, laundry
9am- eats breakfast (tea and biscuits), and cooks food
11am- eats lunch (rice with fish/dhal etc)
3pm- eats same dishes again, and sleeps for 2 hours, watches television
5pm- drinks tea, makes her kids study
10pm- eats dinner (rice with curries)
11pm- Sleeps and wakes up in the middle of the night after 5 hours of sleeping due to low back pain.
PAST HISTORY:
Not a known case of DM, Hypertension, Epilepsy, Asthma, Thyroid disorders, CVA, CAD.
PERSONAL HISTORY:
The patient is housewife by occupation.
Diet - mixed
Appetite- Normal
Bowel and bladder movements -regular
Sleep- Adequate
Addictions - no addictions
SURGICAL HISTORY:
2 previous LSCS in 2009 and 2015.
The 2nd LSCS is followed by HYSTERECTOMY in 2015.
History of a first trimester spontaneous Abortion About 9 yrs ago .D and C done In Local hospital
FAMILY HISTORY:
NO SIGNIFICANT FAMILY HISTORY.
MENSTRUAL HISTORY:
LMP- 18/02/2023
Menstrual cycle- 45/5, Irregular cycles
OBS Formula- P2L2
GENERAL EXAMINATION:
Patient is C/C/C
No signs of pallor, icterus, cyanosis, clubbing, lymphadenopathy, edema.
Vitals:
BP- 130/70mmhg
Temp- Afebrile
PR- 78bpm
RR- 16cpm
SpO2 - 99% @ Room air
SYSTEMIC EXAMINATION:
CVS: S1,S2 heard ,no murmurs
RS: BAE +, no crepts
P/A: soft, non tender, Bowel sound heard
O/E:
Spinal tenderness @ L4 and L5
SLRT- (-ve)
Schobers test- (-ve)
CNS- NFDF
Reflexes- B. T. S. A. K.
Right- 2+ 2+ 1+ 2+ 2+
Left-. 2+ 2+ 1+ 2+ 2+
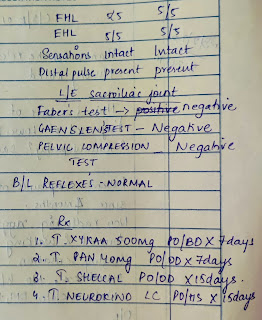
Orthopedic referral done on 23/02/23-








Comments
Post a Comment